How to utilise your own immune system in cancer treatment
According to the theory of anti-tumor immune surveillance, the immune system can neutralise most tumor cells before the disease ever develops. Despite this, nearly 90,000 cancer patients are diagnosed in the Czech Republic every year. The research of the Laboratory of Tumor Immunology at the Institute of Microbiology of the CAS is contributing to the search for new treatment options making use of the immune system itself. We covered the topic in the CAS magazine A / Věda a výzkum. This story is being featured on the occasion of World Cancer Day, which falls on Saturday, 4 February this year.
As recently as the 1980s, being diagnosed with advanced malignant melanoma was still considered practically a death sentence. Nowadays, medical science can cope with skin cancer (as malignant melanoma is popularly known) in certain cases and makes use of various treatment methods. Some of these are based on stimulating the patient’s immune system.
In the late 1990s, one of the first approved immunotherapy drugs, Proleukin, raised a lot of hopes. “When [the drug] worked, it worked well. About 15% of people treated went into remission, and of those, up to 8% survived for years, even decades,” recalls oncologist Jonathan Drachman in the journal of the American Chemical Society, Chemical & Engineering News.
However, it was no miracle cure, due to the very serious side effects and impractical administration. Infusions of the drug had to be administered in a hospital under direct medical supervision – always several high doses over a few hours during several days. It appeared as though Proleukin, a drug that uses a signalling molecule (glycoprotein) in the immune system called interleukin-2 (IL-2 for short), would not be able to be used on a large scale after all.
But the 15% remission rate for a cancer with an otherwise nearly 100% mortality rate was not negligible, and researchers and doctors still decided to puzzle over how to modify IL-2 to avoid the serious side effects while increasing its anti-cancer efficacy.
Even today, many research teams around the world are working on ways to improve IL-2. One of them can also be found in Prague, in the Laboratory of Tumor Immunology of the Institute of Microbiology of the CAS.
Scepticism or hope?
“We started working on this research about fifteen years ago, after I had returned from my postdoc fellowship in California. I spent two years there in the laboratory of Professor Jonathan Sprent who, among other things, was also working on IL-2 at the time,” says Marek Kovář, Head of the Laboratory of Tumor Immunology.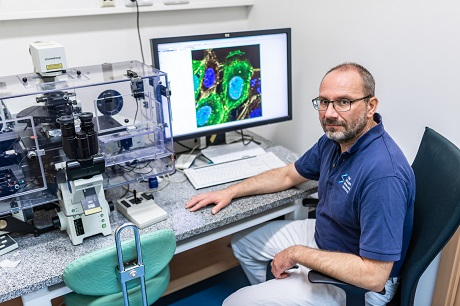 Marek Kovář, Head of the Laboratory of Tumor Immunology at the Institute of Microbiology of the CAS.
Marek Kovář, Head of the Laboratory of Tumor Immunology at the Institute of Microbiology of the CAS.
While the cytokine IL-2 is a relatively small molecule, it plays a very important role in the regulation of the immune system. It can stimulate certain immune cell populations, e.g., activated T lymphocytes, memory CD8+ T lymphocytes, and NK (natural killer) cells. However, it also has the capability to inhibit the immune response by increasing the number and functional activity of regulatory T cells.
This dual function makes it theoretically possible to use IL-2 for cancer therapy as well as for the treatment of autoimmune diseases or, for instance, transplantations. In the former case, it is desirable to increase the stimulatory activity of IL-2 for CD8+ T lymphocytes and NK cells and to suppress the stimulatory activity for T regulatory cells; in the latter case, the opposite is true. In theory this looks promising, so the question is why IL-2 is not being used more in medicine.
One of the many problems is that IL-2 has a very short half-life – that is, it disappears from the body very quickly (in a matter of tens of minutes) after being administered. Thus, for IL-2 to have any significant therapeutic effect, huge amounts of it must be injected into the body, but this can give rise to life-threatening side effects.
Kovář also points out the toxicity of immunotherapy using IL-2. “Due to the application of high doses of IL-2, capillaries in certain organs dilate and the connections between endothelial cells get disrupted. It has very serious consequences, including pulmonary edema, which can be fatal. Immunotherapy with IL-2 is also quite hepatotoxic, which means it can cause liver dysfunction,” he explains.
The taming of a signaling molecule
At the beginning of the millennium, Jonathan Sprent’s team, which Kovář was a part of, succeeded in demonstrating that when IL-2 complexes are formed with antibodies specific for IL-2 (IL-2 mAb), much higher biological activity is achieved compared to IL-2 alone. Among other things, the half-life of IL-2 is significantly prolonged by the immune complexes. “What is even more interesting, though, is that different monoclonal antibodies recognise different parts of the IL-2 molecule – the so-called epitopes – and thus form complexes with IL-2 with selective biological activity either for potential effectors, i.e., CD8+ T lymphocytes and NK cells, or for T regulatory cells,” Kovář says.
The advantages of using IL-2/IL-2 mAb complexes versus IL-2 alone are therefore evident: the possibility of administering significantly lower doses and relatively selective stimulation of those immune cell populations for which it is desirable given the particular disease. The results of the study were published in the prestigious journal Science in 2006.
Subsequent tests on animal models focused on the effectiveness of cytokine-antibody complexes for potential clinical applications, finding that the principle works not only for IL-2, but for other cytokines such as IL-4 and IL-7 as well.
Kovář’s team continues to work with IL-2/IL-2 mAb complexes in the lab and is trying to uncover more knowledge about them. The team is testing IL-2/IL-2 mAb complexes in combination with other types of immunotherapy, such as blockers of certain inhibitory molecules on T lymphocytes. The researchers are also looking into chemotherapy with so-called polymeric drugs, which have lower immunosuppression than conventional chemotherapy and are therefore much better suited for combination chemoimmunotherapy. Taking it to the next qualitative level is the effort to prepare cytokine-mAb complexes as fusion (chimeric) proteins.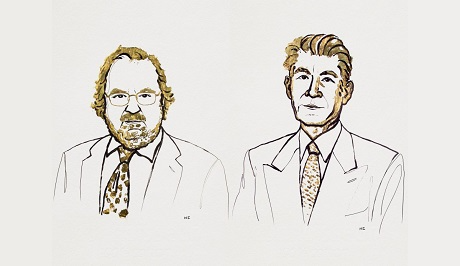 Immunotherapy is a fundamental approach to cancer treatment, and was awarded the 2018 Nobel Prize in Physiology or Medicine. It was won by American researcher James P. Allison and his Japanese colleague Tasuku Honjo.
Immunotherapy is a fundamental approach to cancer treatment, and was awarded the 2018 Nobel Prize in Physiology or Medicine. It was won by American researcher James P. Allison and his Japanese colleague Tasuku Honjo.
From test tube to the patient’s bedside
In addition to IL-2/IL-2 mAb complexes, the Laboratory of Tumor Immunology (Institute of Microbiology of the CAS) is also researching the cytokine IL-15, which doesn’t differ much from IL-2. It has similar biological activity and structure – they both share two receptor subunits (beta and gamma). “With Professor Sprent, we were also working with IL-15. Back then we discovered that the biological activity of IL-15 can be significantly potentiated by having the extracellular part of the alpha subunit of its own receptor (IL-15Rα) bind to it,” Kovář explains.
The results of this study were published in the journal PNAS in 2006. The IL-15 molecule, or rather, its complex formed with IL-15Rα, is being further developed by several research teams and pharmaceutical or biotech companies around the world. One of these includes SOTIO Biotech, which is based in Prague. Its aim is to develop and research various immunotherapeutics useful for the treatment of cancer. Among others, they consider the substance called SOT101, which consists of IL-15 and IL-15Rα, as promising.
Kovář’s team is working on testing SOT101, which is now in the second phase of clinical trials. “So far, all indications are that it works very well, the therapeutic effect in mouse tumor models is excellent, but even that is no guarantee that the substance will actually become a clinically used drug. A great deal of additional experimental research is still needed to gain enough knowledge about this potential form of immunotherapy,” the researcher points out.
 Marek Kovář’s team is currently testing SOT101, a potential immunotherapeutic drug for cancer treatment.
Marek Kovář’s team is currently testing SOT101, a potential immunotherapeutic drug for cancer treatment.
The future of SOT101 rests with the biotech company involved and, above all, will depend on the decision of the regulatory authorities to allow further phases of testing or not. The journey of a drug from test tube to the patient’s bedside can take well over a decade and statistically, only a small proportion of drugs that enter clinical trials ever succeed.
“This research is one for the long haul. The chances of any one given researcher making a breakthrough discovery are awfully small. On the other hand, advancements in biomedical fields over the last decade or two have been astonishing,” Kovář adds, recalling his former supervisor from the U.S., Jonathan Sprent. “He originally worked as a doctor, treating children with leukemia. In his youth, leukemia was considered a deadly disease, and the vast majority of child patients were dying. The situation today is that nine out of ten children who get some kind of acute childhood leukemia live to adulthood – that is, if they live in countries with advanced health systems.”
However, childhood leukemia requires a different kind of treatment, whereas IL-2 is now mostly used for metastatic malignant melanoma or kidney cancer, and in those cases, the prognosis is not very positive. “Our research is mainly concerned with different types of cancers that are predominantly found in older people. And it certainly makes sense, despite the fact that the prospects are not bright. I am glad to be doing work where we have the opportunity to come up with something new,” Kovář concludes.
Publication: Onur Boyman, et al., Selective Stimulation of T Cell Subsets with Antibody-Cytokine Immune Complexes, Science (2023). DOI: 10.1126/science.1122927.
Original Story Source: Columbia University, New York

 Alerts Sign-up
Alerts Sign-up