Vaccine Delivers A Boost To T Cell Therapy
The new strategy may enable engineered T cells to eradicate solid tumors such as glioblastoma.
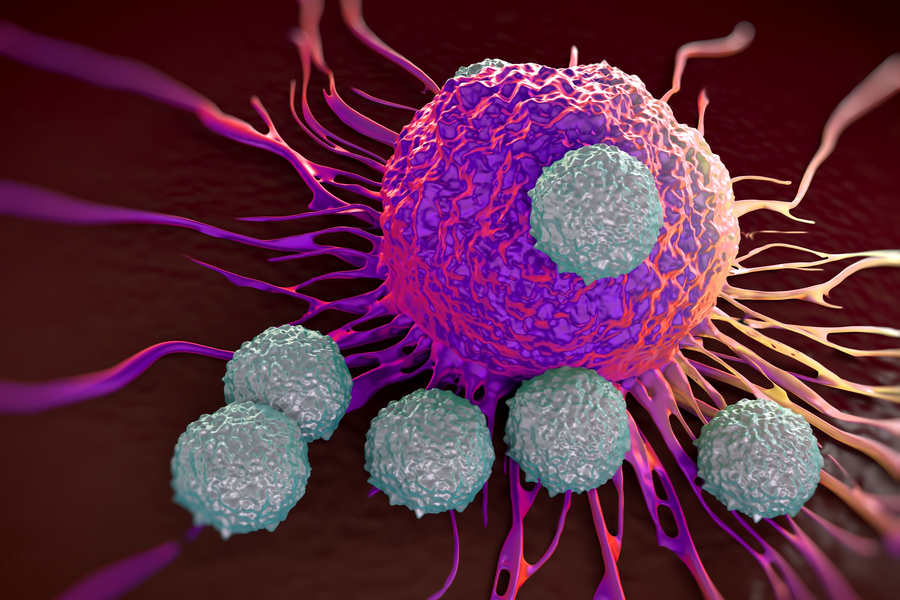 Engineering T cells to destroy cancer cells has shown success in treating some types of cancer, such as leukemia and lymphoma. However, it hasn’t worked as well for solid tumors.
Engineering T cells to destroy cancer cells has shown success in treating some types of cancer, such as leukemia and lymphoma. However, it hasn’t worked as well for solid tumors.
One reason for this lack of success is that the T cells target only one antigen (a target protein found on the tumors); if some of the tumor cells don’t express that antigen, they can escape the T cell attack.
MIT researchers have now found a way to overcome that obstacle, using a vaccine that boosts the response of engineered T cells, known as chimeric antigen receptor (CAR) T cells, and also helps the immune system generate new T cells that target other tumor antigens. In studies in mice, the researchers found that this approach made it much more likely that tumors could be eradicated.
“This vaccine boosting appears to drive a process called antigen spreading, wherein your own immune system collaborates with engineered CAR T cells to reject tumors in which not all of the cells express the antigen targeted by the CAR T cells,” says Darrell Irvine, the Underwood-Prescott Professor with appointments in MIT’s departments of Biological Engineering and of Materials Science and Engineering, and a member of MIT’s Koch Institute for Integrative Cancer Research and the Ragon Institute of MGH, MIT, and Harvard.
Irvine is the senior author of the study, which appears today in Cell. The lead author of the paper is Leyuan Ma, a former postdoc at the Koch Institute and currently an assistant professor of pathology and laboratory medicine at the University of Pennsylvania School of Medicine.
Engineered T cells
The U.S. Food and Drug Administration has approved several types of T cell treatments for blood cancers. These treatments are based on CAR-T cells, which are engineered to display receptors that can recognize a specific antigen found on cancer cells.
To try to adapt this kind of treatment to glioblastoma, a type of brain cancer, researchers have designed CAR-T cells that target a mutated version of the EGFR receptor. However, not all glioblastoma cells express this antigen, and when attacked by CAR-T cells, some glioblastoma cells respond by halting production of the target antigen.
In a 2019 study, Irvine and his colleagues enhanced CAR-T cells’ effectiveness against glioblastoma by delivering a vaccine to mice shortly after the engineered T cells were administered. This vaccine, which carries the same antigen targeted by the CAR-T cells, is taken up by immune cells in the lymph nodes, where the CAR-T cells are exposed to it.
In that study, the researchers found that this vaccine boost not only helped the engineered CAR-T cells attack tumors, but it had another, unexpected effect: It helped to generate host T cells that target other tumor antigens.
This phenomenon, known as “antigen spreading,” is desirable because it creates populations of T cells that, working together, can fully eradicate tumors and prevent tumor regrowth.
“That would be exactly the kind of thing that could help you deal with the antigen heterogeneity of solid tumors, because if you primed host T-cells to attack other antigens, they may be able to come in and kill the tumor cells that your CAR-T cells cannot,” Irvine says.
An immune boost
In their new study, the researchers wanted to explore how that additional T-cell response becomes activated. They used the same type of CAR-T cells from their 2019 study, which are engineered to target mutant EGFR, and the same vaccine. The mice in the study were given two doses of the vaccine, one week apart.
The researchers found that in these boosted mice, metabolic changes occurred in the CAR-T cells that increased their production of interferon gamma, a cytokine that helps stimulate a strong immune response. This helps the T cells to overcome the immunosuppressive environment of the tumor, which normally shuts down any T cells in the vicinity.
As the CAR-T cells killed tumor cells expressing the target antigen, host T cells (not the engineered CAR-T cells) encountered other antigens from those tumor cells, stimulating those host T cells to target those antigens and help destroy tumor cells.
Without that host T cell response, the researchers found, tumors would regrow even if the CAR-T cells destroyed most of the original tumor cells. This happens because tumor cells treated with CAR-T cells often stop producing the antigen targeted by the engineered cells, allowing them to evade those cells.
Tumor eradication
The researchers then tested their approach in mice with tumors that had different levels of the target antigen. They found that even in tumors where only 50 percent of the tumor cells expressed the target antigen, about 25 percent of the tumors could still be eradicated, by a combination of CAR-T cells and host T-cells.
The success rate was higher for tumors with greater levels of the target antigen. When 80 percent of the tumor cells expressed the antigen targeted by CAR-T cells, tumors were eliminated in about 80 percent of the mice.
The technology used in this study has been licensed to a company called Elicio Therapeutics, which is working on developing it for potential testing in patients. In this study, the researchers focused on glioblastoma and melanoma, but they believe it could potentially be used to combat other types of cancer as well.
“In principle, this should apply to any solid tumor where you have generated a CAR T-cell that could target it,” Irvine says.
The researchers are also working on ways to adapt CAR-T cell therapy so that it can be used to attack tumors for which no targetable antigens have been identified.
The research was funded by the National Institutes of Health, the Marble Center for Cancer Nanomedicine at the Koch Institute, an ASPIRE Award from The Mark Foundation for Cancer Research, an American Cancer Society postdoctoral fellowship, the Cell and Gene Therapy Collaborative at the Children’s Hospital of Philadelphia, the W.W. Smith Charitable Trust, and a Koch Institute Support (core) Grant from the National Cancer Institute.
Publication: Leyuan Ma, et al., Vaccine-boosted CAR T crosstalk with host immunity to reject tumors with antigen heterogeneity, Cell (2023) DOI : 10.1016/j.cell.2023.06.002
Original Story Source: Massachusetts Institute of Technology

 Alerts Sign-up
Alerts Sign-up